Systematic Review of Ketogenic Diet and Cognitive Disorders
- Review
- Open Access
- Published:
Are ketogenic diets promising for Alzheimer's disease? A translational review
Alzheimer's Research & Therapy volume 12, Article number:42 (2020) Cite this article
Abstract
Background
Brain amyloid deposition and neurofibrillary tangles in Alzheimer's disease (Advertising) are associated with complex neuroinflammatory reactions such as microglial activation and cytokine production. Glucose metabolism is closely related to neuroinflammation. Ketogenic diets (KDs) include a high amount of fat, low carbohydrate and medium-concatenation triglyceride (MCT) intake. KDs atomic number 82 to the production of ketone bodies to fuel the encephalon, in the absence of glucose. These nutritional interventions are validated treatments of pharmacoresistant epilepsy, consequently leading to a better intellectual development in epileptic children. In neurodegenerative diseases and cerebral pass up, potential benefits of KD were previously pointed out, just the published evidence remains scarce. The main objective of this review was to critically examine the evidence regarding KD or MCT intake furnishings both in AD and ageing animate being models and in humans.
Main trunk
We conducted a review based on a systematic search of interventional trials published from January 2000 to March 2019 found on MEDLINE and Cochrane databases. Overall, 11 animal and xi human studies were included in the present review. In preclinical studies, this review revealed an improvement of cognition and motor role in Advert mouse model and ageing animals. Nonetheless, the KD and ketone supplementation were also associated with significant weight loss. In human being studies, nearly of the published articles showed a pregnant improvement of cognitive outcomes (global cognition, memory and executive functions) with ketone supplementation or KD, regardless of the severity of cognitive impairments previously detected. Both interventions seemed acceptable and efficient to achieve ketosis.
Decision
The KD or MCT intake might be promising means to modify cerebral symptoms in AD, especially at the prodromal stage of the disease. The need for efficient affliction-modifying strategies suggests to pursue further KD interventional studies to assess the efficacy, the adherence to this diet and the potential adverse furnishings of these nutritional approaches.
Background
Carbohydrates represent the primary energy source for the brain. Nonetheless, when glucose is not readily bachelor (e.thousand. starvation), a metabolic switch occurs in favour of ketone bodies (KB), normally released by the liver. The diets specifically designed for KB production are called ketogenic diets (KDs) [one, 2]. They are the get-go and only nutritional interventions that enabled a significant reduction in the incidence of seizures in pharmacoresistant epilepsy [3] or in chronic cluster headaches [four]. The core characteristics of the KD are the association of a high corporeality of fatty, with depression carbohydrate intake, commonly a macronutrient ratio of fat to poly peptide and carbohydrate combined equal to 3–4:one. Alternative KDs were developed using ketone supplementation (KS), in which fats are provided with medium-chain triglyceride (MCT) intake. Their common objective is to achieve ketosis, leading to reduced insulin secretion and glycaemia within 48 h, as well equally a shift in the brain's metabolism [ii].
In Alzheimer's illness (Advertizing), it is described numerous interrelations betwixt abnormal glucose metabolism and the occurrence of brain lesions. Outset, Ad could be a partial issue of insulin resistance, which affects insulin signalling and favours in the encephalon abnormal deposition of β-amyloid peptide (Aβ) and phosphorylated tau (pTau) accumulation, leading in turn to cognitive decline [five]. Furthermore, the expression of apolipoprotein Eastward allele 4 (APOE4) is a mutual hazard factor for Ad and for type 2 diabetes suggesting a common pathophysiological background [6]. As demonstrated by fluorodeoxyglucose positron emission tomography (FDG-PET), abnormal brain glucose metabolism in the temporal and parietal lobes occurs from the earliest stages in Advert creature models and Advertisement patients but as well in asymptomatic individuals at risk for AD [7]. Interestingly, these hypometabolic regions are nevertheless able to take upward KB, even though they can no longer utilize glucose [8].
At the cellular level, several KD neuroprotective effects have been observed, linked to various mechanisms: (i) reduction of the concentration of several excitatory neurotransmitters (e.k. glutamate) [9], (ii) stabilization of synaptic functions due to enhanced mitochondrial biogenesis [10] and (three) reduction of reactive oxygen species generation and increment adenosine triphosphate availability [11]. Moreover, KB have specific protective effects against cerebral Aβ toxicity and cell harm as shown in rat cultured hippocampal neurons [12]. Aβ can induce neuroinflammation, which is a current therapeutic target in AD. KD could modulate Aβ toxicity by promoting the action of endogenous anti-inflammatory molecules such as peroxisome proliferator-activated receptor γ, leading to a decreased systemic inflammation [13].
These observations, likewise equally the current lack of success of anti-Advertisement therapies or nutritional interventions to change the course of AD, suggest that KD or KS might be of therapeutic interest in these patients. A potential benefit of KDs in AD was already claimed in media and some scientific reports [14, 15]. However, every bit few works take brought well-nigh a critical review of existing data, we hereby propose a comprehensive and translational review of KD efficiency in both preclinical and clinical AD or ageing studies. Thus, the main objective of this review was to assess the effects of ketogenic interventions on clinical and metabolic outcomes (east.g. cognitive function, brain metabolism) or Advertizement biomarkers, both in experimental animals and in humans. Nosotros volition as well examine the potential side effects of ketogenic interventions in these populations, in terms of nutritional change and adverse furnishings.
Research process
We performed a systematic search in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16]. We identified all published manufactures between January 2000 and March 2019 on MEDLINE and Cochrane databases using the Medical Bailiwick Heading (MeSH) terms "ketogenic diet" or "medium-concatenation triglyceride" and contrasted combinations of the following terms: "Alzheimer's disease", "Alzheimer", "cognition" and/or "retentiveness". We only included interventional studies using either KD or KS. We take excluded studies published in languages other than English, focusing on KD diet furnishings in diseases other than Advertizing or performed in cellular models. Titles and abstracts were the base of the initial screening. We evaluated the eligibility of selected articles after full-text readings. We too examined all papers cited in the selected manufactures. We added additional references, based on their originality and/or relevance regarding the scope of this review. Information extraction was performed by vi authors (ML, BP, EC, FML, JH, CP), using a standardized extraction form. This tool assessed the study design, population (number of animals/participants, fauna model/ageing individuals or Advertizing patients), type of ketogenic intervention, outcomes (e.chiliad. biological endpoint, clinical endpoint, neuroimaging endpoint), follow-up duration, nutritional changes and potential side effects due to the intervention. This search was carried out in April 2019.
Results
Amidst ane hundred forty-six selected papers, nosotros identified 84 interventional studies. Two additional interventional studies were found through the bibliography of the relevant animal studies papers. In total, 22 (11 animal studies and 11 human studies) were considered relevant for the present review. Nosotros summarized details of animal and human studies in Tables 1 and ii, respectively. Effigy 1 outlines the results of the systematic searches.
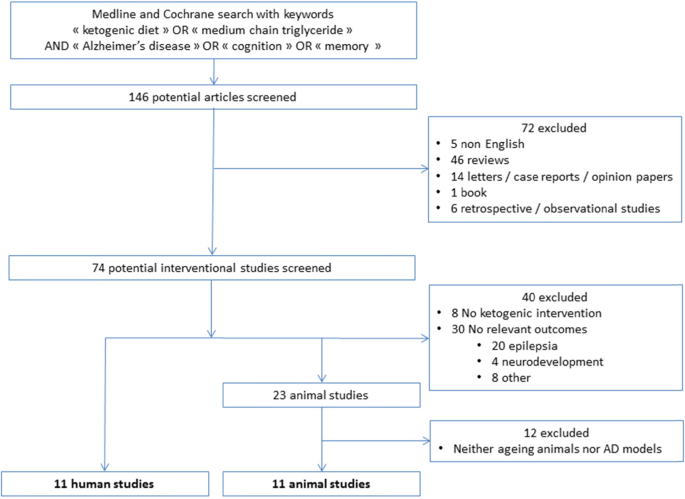
Flow diagram of studies selection
Preclinical studies
Two types of interventions were used: KD (N = 7) either advertisement libitum or calorie-controlled, and KS (N = iv), compared to control diet or placebo, respectively. Fifty-fifty if the total number of animals varied from i study to the other (from sixteen to 65 with a hateful of 48.v ± 5.2 animals), the number in each treatment group was nearly the same. Overall, baseline age at the start, species or Advert model type, sex activity and follow-up elapsing varied between studies.
Ageing animals
Five studies assessed ketogenic interventions in ageing animals. The hateful historic period at baseline varied depending on the studied species: 9 years for beagle dogs (Northward = 1), higher up 20 months for wild-type (WT) rats (Due north = three) and 12 months for WT mice (N = i). Simply ii studies out of five compared young (iv-month-old WT rats) vs ageing animals [20, 21]. Three studies used only ageing male person rodents [xx, 23, 27] whereas two other studies compared the effect of KD/KS on ageing males and females [21, 24]. The follow-upwards elapsing was different co-ordinate to species: 8 or 12 weeks for WT rats [twenty, 21, 27], 32 weeks for beagle dogs [24] and 72 weeks for former WT mice on which the effect of KD on life bridge was evaluated [23].
Alzheimer's disease beast models
6 studies included unlike Advertisement mouse models, based on the amyloid pour hypothesis. Briefly, 3xTgAD mice [22, 25], APP/PS1 mice [17, xviii], APP [V7171] mice [26] and APP+PS1 [19] mice were used. Interestingly, Brownlow et al. choose to compare an amyloid-based AD model (APP+PS1 mice) and a tau-based AD model (Tg4510 Advert mice) [19]. One of these studies used but female Ad mouse model (APP [V7171]) [26]. Regarding baseline age, 3xTgAD mice were older (viii.five months) than APP [V7171] (iii months), APP/PS1 (between 1 and 3 months) and APP+PS1 and Tg4510 mice (5 months). The follow-up duration varied from four to 32 weeks (mean 17 ± 5.05 weeks) without a link between elapsing and a blazon of AD model.
Outcomes and results
The following objectives were assessed: efficacy on knowledge and/or motor functions (N = 3 assessing both, Northward = v assessing noesis only, Due north = 1 assessing motor part only), impact on neuropathological Advertizing lesions (N = five), KD safety (Due north = 1) and weight variations (N = 9). Eight studies (one in former WT mice, two in young vs ageing WT rats and v in Advertizement mouse models) evaluated multiple outcomes.
In ageing animals
Three studies evaluated the effects of KD in ageing animals, either on safety and cognition [23], weight and neurotransmitter function [20] or cognition/motor function and neurotransmitter part [21].
Effects of KD/KS on life expectancy and mortality
Only Newman et al. conducted a long-term written report of KD. They showed that KD was able to reduce mid-life mortality but without improving maximum lifespan in old C57Bl6 WT mice [23].
Cognitive and motor impact of KD/KS
Four studies evaluated the cognitive impact of KD and showed a positive effect on knowledge, in ageing animals [twenty, 23, 24, 27]. This effect was observed with several KD formulae (2 calorie-controlled KD, two KS). This result suggests that brain metabolism can shift towards the use of KB, regardless of the kind of ketone-oriented diet used, with potential cognitive gain. Similarly, motor performances were improved in all studies, regardless of potential associated cerebral benefits. These results are consequent with many mouse studies demonstrating that keto-accommodation enhanced the capacity to transport and metabolize fat as well as motor abilities and recovery [39,40,41].
Mechanisms underlying cerebral furnishings of KD and KS
Hernandez et al. studied the effect of KD on transport protein expression in the encephalon of ageing mice, notably vesicular glutamate and gamma-aminobutyric acid (GABA) transporters [20, 21]. They observed that KD advertising libitum was able to reverse the age-dependent decrease of vesicular GABA transporter expression in the hippocampus and in the prefrontal cortex. This result could be linked to the known effect of KD in epilepsy [3]. Indeed, KD enhances GABA vesicular filling which maintains an inhibitory feedback associated with the beneficial effect of KD. 1 can also hypothesize that this effect on GABA may have a potential anxiolytic effect. Interestingly, the authors described a like reversal event on the age-dependent decrease of vesicular glutamate transporter expression that was not restricted to the hippocampus.
In improver, Wang and Mitchell described that KS is associated, in old WT rats, with an increase in insulin receptor 1 levels and Akt phosphorylation and a subtract in ribosomal protein S6 kinase phosphorylation [27]. KS consequence on this pathway is associated with increased ube3a expression that notably plays a role in synaptic stabilization. Conversely, Newman et al. identified a downregulation of the insulin pathway in old WT mice fed with KD advert libitum [23]. The conflicting results of the two studies can exist due to the discrepancies concerning the elapsing of nutrition (8 vs 72 weeks) and/or the baseline historic period of the animals (21 vs 12 months). So far, data are not sufficient to conclude on the mechanisms responsible for the cognitive impact of KD/KS in ageing brain or whether there even is an bear upon. Yet, if there is an consequence of KD/KS on knowledge, one outset hypothesis might be synaptic protection through neurotransmitter pathway and/or synaptic stabilizations.
Furnishings of KD/KS on weight
Two studies [20, 27] showed a significant weight loss while no body weight modifications were observed in the two others [23, 24]. Among the four, but Hernandez et al. observed a meaning weight loss despite a calorie-controlled KD. This effect was specific to old WT rats, but an unexpected fat mass reduction was observed both in young and old WT rats [xx].
In Alzheimer's disease creature models
In details, v studies using Ad mouse models assessed knowledge and/or motor part together with histological data [17,18,xix, 22, 26] while one assessed both impacts on weight and histology [24].
Cognitive and motor impact of KD/KS
Two studies assessed the cognitive impact of KD in Advertizing mouse models [17, 22]. Mice merely showed a cerebral gain in the latter study, in which triheptanoin was added to KD. Co-ordinate to the authors, the cerebral proceeds was likely to event from an enhanced mitochondrial function, due to triheptanoin supplementation [17]. In the other written report, motor coordination was significantly improved in the KD group.
Effects of KD/KS on AD pathological lesions
Five studies specifically assessed the changes in Aβ and/or tau deposition in Ad mouse models [17,eighteen,19, 22, 26]. Kashiwaya et al. and Van der Auwera et al. described a decrease in Aβ deposition in the brain of KD-fed female APP [V7171] and male 3xTgAD mice, respectively. In addition, Kashiwaya et al. reported a significant reduction of abnormal pTau labelling in the hippocampal neurons of 3xTgAD mice under a calorie-controlled KD. On the other hand, Aso et al., Beckett et al. and Brownlow et al. failed to report any meaning improvement in encephalon amyloid load after KD in APP/PS1 [17, 18], APP+PS1 and Tg4510 (tau) AD mouse models [nineteen].
Several factors or combined factors could explain this discrepancy, only we will focus on the two mains: (i) type of diet and/or its elapsing and (ii) blazon of Advert model and time course of lesion onset. Regarding diet, the duration of the intervention might have played a function in the observed discrepancy. Indeed, this result on Aβ aggregating and pTau pathology in 3xTgAD mice was described when an animal received a KS for 32 weeks [22]. This result may also exist due to a specific therapeutic event of the synthetic ketone ester (R)-iii-hydroxybutyrate-(R)-1,3-butanediol monoester, administered as a dietary supplement.
The option of an Advert mouse model is crucial in this setting. All Ad mouse models used are based on the overexpression of Aβ, but they differed in terms of the type and/or the pathological fourth dimension course of the disease. Thus, promoters regulating the mutated factor expression are model-dependent so is Aβ production and accumulation. Ad models with high Aβ production and accumulation similar 3xTgAD (combining amyloidopathy and tauopathy) or APP [V7171] (early-onset familial AD) were the ones in which the effect of the ketogenic interventions was observed [22, 26]. KD, like calorie-restricted diet, might induce insulin-degrading enzymes directed against Aβ [42]. Accordingly, an issue on Aβ aggregating based on degradation is easier to discover in animals with college Aβ accumulation. In addition, the time course of the lesions depends on model types. Therefore, if the aim of the intervention is to evaluate the effect on Aβ load, the intervention has to accept into account this parameter. For instance, in APP/PS1 mice, soluble Aβ became detectable from iii months onward and amyloid plaques appeared at ix months. Studying the effect of KD/KS before those milestones or with an early endpoint may lead to the absence of observed effect [17, 18]. It is also interesting to note that the type of promoter also affects the magnitude of Aβ load. For example, the prion protein promoter, present in APP+PS1 and APP/PS1, is responsible for a more widespread and less selective Aβ expression than others [43]. Localization of amyloid encephalon load may differ from i animal model to the other, and analyzing methods have to be adapted. Thus, analysis restricted to specific brain regions (e.g. Aβ immunochemical labelling in the prefrontal cortex or hippocampus [24]) seems to be more efficient than global analysis (e.g. whole-brain enzyme-linked immunosorbent analysis against full Aβ and APP C-terminal [25]).
Regarding other abnormal features in models of Advertising, Aso et al. showed a reduction of neuroinflammation afterwards intake of KD + triheptanoin in APP/PS1 mouse that was not observed in APP/PS1 mouse fed with KD just and thus might be specific to triheptanoin supplementation [17]. Pawlosky et al. observed that KS induced a reduction of the free radical insult against hippocampal proteins and modified both α- and β-secretase expression levels (college and lower respectively) in hippocampal just not in cortical lysates [25]. KS is able to reduce the levels of hippocampal BACE 1, a key enzyme in the production of Aβ peptide, and this finding could explain the reduction of amyloid load.
Overall, KD and KS seemed to be able to reduce Aβ and pTau load also every bit neuroinflammation, especially in aggressive mouse models treated for a long time. In some models, those neuropathological effects were associated with improvement of cognitive and/or motor functions. While the underlying mechanisms remain to exist elucidated, these observations support the hypothesis that KD/KS might have definite therapeutic deportment on Ad abnormal biological pathways.
Effects of KD/KS on weight
Four studies, using various methodologies, observed a pregnant weight loss [18, 22, 25, 26], while no body weight modifications were observed in the concluding one [19]. Thus, while these studies used variable cloth and approaches, most of them institute a reproducible weight loss induced past KD or KS. However, details are lacking to depict definite conclusions on the mechanisms of this weight loss and its consequences on the condom of this approach. In that location was no reported association of weight loss to cognitive change in these studies.
Clinical studies
Full general characteristics of the studies
Included humans studies (North = 11) are presented in Tabular array ii. They involved either ageing subjects with or without mild cognitive impairment (MCI) (North = 6; mean age 66.1 to 75.4 years onetime; hateful Mini-Mental Condition Examination (MMSE) score at baseline 17.i to 27.1) or individuals with AD dementia based on clinical diagnostic criteria such as the Diagnostic and Statistical Manual of Mental Disorders-IV or the National Institute of Neurological and Communicative Diseases and Stroke/Alzheimer's Illness and Related Disorders Clan (N = 5). In addition, these studies comprised inconsistent sexual activity ratios (30 to 66% of male person). Five of them indicated an boilerplate level of education betwixt 12.five and 15.three, and only one provided information near the ethnic groups of the written report population (generally Caucasians in 91%).
Thus, participants showed various degrees of cerebral functioning among studies, from normal ageing people to moderate dementia. Two studies did not specify the degree of cognitive impairment of their participants [33, 36]. I can observe that the use of Aβ or tau biomarkers, highly recommended for increasing diagnostic accuracy, was non mentioned in these studies. APOE genotyping was performed in iv studies only [28, 30, 37, 38].
Regarding nutritional interventions, two studies used a classic KD arroyo while xi relied on KS using MCT. Of note, KS protocols differed much in composition and daily dose (twenty to 56 thousand of MCT per day). 2 studies had a crossover design [29, 38] while one did not include a control group [31]. The 7 remaining studies were randomized controlled trials. The number of individuals included varied among studies from 6 to 152 (hateful 31.iii ± 38.two). Likewise, the follow-upwardly durations were rather short and heterogeneous, from 0 to 26 weeks (mean 11.2 ± 9) including iii studies examining the immediate upshot, the same mean solar day as the clinical and cognitive examination of KS [28, xxx, 37, 38].
None of the studies included in this review provided details on patients' medical conditions. Apart from cerebral damage, comorbidities are likely to modulate the efficacy or the adhesion to KD or KS. For case, in patients with type two diabetes, very stringent KD may not be sustainable over long-term, although there is no formal contraindication to it [44]. Too inflammatory diseases, mood disorders, chronic pain and polypharmacy may change the nutritional status of the individuals, as well as the prophylactic of a high-fat diet. Moreover, only Abe et al. presented its exclusion criteria: subjects with body mass index < 23 kg/g2 or major organ dysfunction [32]. Altogether, this impairs the external validity of the studies and pleads for new studies that would appraise the interaction betwixt comorbidities and KD/KS in patients.
Outcomes
All studies only one assessed cognitive changes after KS or KD. One study focused on cognitive changes and the feasibility of long-term KS in cognitively impaired individuals [29]. However, the instruments used to assess cognitive outcomes were inconsistent among studies. Five studies used the Mini-Mental Condition Test [28, 31, 32, 34, 38], and four of them utilized the Alzheimer Disease Assessment Scale (ADAS-cog) [31, 35, 37, 38]. Two studies used a neuroimaging (PET) endpoint: regional cerebral claret flow [xxx] or [11C]-acetoacetate tracer [28].
Metabolic effects of KD/KS in cognitively impaired patients and older adults
Nine studies out of eleven monitored the plasma levels of KB to brand sure that participants really accomplished ketosis. Thus, the authors were able to demonstrate that ketosis was speedily and efficiently reached in all the studies, regardless of the type of intervention. Even so, but v studies examined the changes in nutritional status or body composition in patients under KS/KD [28, 31, 32, 35, 36]. Krikorian et al. highlighted a mean weight loss of four kg per individual after half-dozen weeks, in MCI adults under KD as compared to patients nether control nutrition [36]. This finding is consistent with the results of a meta-assay showing that KD is commonly associated with weight loss, due to reduced total calorie intake [45].
Three other studies did not show any significant weight change with KS [28, 31, 35]. Interestingly, Abe et al. observed that participants improved their muscle mass and function [32]. Of annotation, those subjects received vitamin D and leucine in addition to the nutritional intervention, which may have contributed to this anabolic outcome.
Finally, simply four studies reported on the side furnishings of KS/KD [28, 31, 36, 37], including the study by Henderson et al. that described gastrointestinal symptoms (49%), which led to treatment discontinuation (23% in the intervention grouping).
Cognitive effects of KD/KS
Autonomously from the Torosyan et al. report (no clinical endpoint) [thirty], the majority of the studies (6 out of x) observed significant cognitive improvements in the intervention groups (KS or KD), regardless of participants' cognitive status (from MCI to severe Advertising patients). On the other hand, the three remaining studies did not study whatever significant effect on cognition [28, 34, 35]. Cunnane et al. previously mentioned that given a choice between glucose and ketones, neurons would rather swallow the latter [8]. As well, even though brain-imaging studies revealed that encephalon utilization of glucose declines in early AD, KB utilization does not [46]. The results of the 2 PET imaging studies evaluated for this review were consistent with these findings [28, 30]. Interestingly, Torosyan et al. showed a long-term increase in brain metabolism afterward KS in non-APOE4 individuals [30]. This is in line with the results of three studies included in this review that highlighted better efficiency of KS in non-APOE4 subjects [30, 37, 38]. There is also an established relationship between APOE4 genotype and brain amyloid deposition. It is noteworthy to say that in the PREDIMED-NAVARRA randomized-controlled trial, non-APOE4 genotype was associated with greater improvement of the MMSE and Clock Drawing Test scores when following a Mediterranean diet rather than a Western-type diet [47]. Thus, the human relationship between APOE4 condition and cerebral effects of metabolic interventions deserves further investigations.
Limitations of the studies
Despite the interesting findings of these 13 studies, many limitations must exist best-selling. First, studies announced highly heterogeneous, in item regarding age, gender ratios or participants' cognitive condition, which all have a pregnant effect on the risk of subsequent cognitive decline. These limitations prevent from drawing robust conclusions about the cognitive benefits of the ketogenic interventions. Some results may also be questionable such as an unexpected cognitive decline measured with the ADAS-cog scale under placebo afterwards only 45 days in MCI individuals whereas in the intervention group, participants maintained their cognitive level [37].
The short follow-upwardly durations and the repeated cerebral assessments are likely to exist responsible for a retest event peculiarly in cognitively intact or MCI individuals. Conversely, patients with mild-to-moderate dementia may exist besides severely impaired to notice benefits from an intervention. This observation was previously raised when discussing the failure of anti-amyloid therapies in AD [48]. Furthermore, all studies aimed at measuring short-term changes in noesis or brain metabolism. The absence of long-term follow-up did non provide any insight into the persistence of cerebral changes after discontinuation of the nutritional intervention. Adhesion to the KD or to KS intake must be advisedly examined as far as long-term nutritional changes are expected. Besides, the monitoring of potential adverse effects is mandatory, specially in AD, since nutritional status is a cardinal predictor of rapid cognitive decline equally well every bit functional limitations [49]. Finally, the small-scale number of studies published then far raises the issue of a potential publication bias every bit negative studies on the furnishings of KS or KD on noesis could not be published.
Conclusion
Despite the growing involvement for KD in AD over the terminal years, simply few interventional studies in animals or humans conspicuously addressed the subject. In preclinical studies, this review pointed out some interesting results such equally comeback of noesis and motor office in some AD mouse model or ageing animals. The mechanisms leading to a benefic effect on knowledge could be due to the (i) modification in neurotransmitter transport pathway and/or synaptic maintenance in ageing WT animals and (ii) improvement of abnormal features (Aβ load or neuroinflammation) in AD mouse models. Notwithstanding, we must go along in mind that KD was initially created (and is still popular) for inducing weight loss in salubrious or overweighed adults. In cognitively impaired subjects, older adults or animal studies, information technology was likewise often associated with a significant weight loss. This consequence could play an adverse outcome on muscle functioning (sarcopenia) or even on cerebral decline. In humans, however the high heterogeneity of the studies and methodological issues discussed above, most of the published studies could suggest improved cerebral outcomes (memory, executive function or global noesis) with KS or KD, regardless of the severity of cognitive harm. Both interventions seemed acceptable for included subjects and show efficacy to achieve ketosis. KD and KS intake both offer different features and potential benefits. They besides present different disadvantages. KD might be difficult to starting time in older adults with modern eating habits and fifty-fifty more difficult to maintain. KS are useful to accomplish ketosis just do not lead to the same metabolic shift, since the brain is still beingness fueled by glucose.
Every bit a decision, the KD might be a promising mode to fight confronting the cognitive symptoms of Advertizing, peculiarly from the prodromal stage of the disease (MCI). Regarding the trunk of evidence discussed above, the hypothesis that KD could postpone cognitive decline in AD should exist explored. Unlike omega-3 supplements or Ginkgo biloba, the ketogenic interventions have not been evaluated yet in large sample randomized controlled trials with sufficient follow-up and structured cognitive and neuroimaging outcomes. Therefore, farther studies are warranted, in detail, in adults with early Ad, not only to appraise the efficiency of the KD on cognitive turn down, but besides to examine the adverse effects (e.g. weight loss, malnutrition) as well as the adherence to the nutrition.
Availability of data and materials
Not applicable.
Abbreviations
- Aβ:
-
β-Amyloid peptide
- Advertizement:
-
Alzheimer'due south disease
- ADAS-cog:
-
Alzheimer Illness Assessment
- ADCS-CGIC:
-
Alzheimer'due south Illness Cooperative Study Scale Clinical Global Impression of Modify
- APOE4:
-
Apolipoprotein E allele 4
- APP:
-
Amyloid precursor protein
- BACE 1:
-
Beta-secretase 1
- cal ctrl:
-
Calorie-controlled
- CD:
-
Control nutrition
- DST:
-
Digit Symbol Exam
- FDG:
-
Flurodeoxyglucose
- FU:
-
Follow-upward
- GABA:
-
Gamma-aminobutyric acid
- GI:
-
Gastro-intestinal
- KB:
-
Ketone bodies
- KD:
-
Ketogenic nutrition
- KS:
-
Ketone supplementation
- MCI:
-
Mild cognitive damage
- MCT:
-
Medium-chain triglyceride
- MeSH:
-
Medical discipline heading
- MMSE:
-
Mini-Mental Status Examination
- MoCA:
-
Montreal Cognitive Cess
- PET:
-
Positron emission tomography
- PS:
-
Presenilin
- pTau:
-
Phosphorylated tau
- RCT:
-
Randomized controlled trial
- TMT:
-
Trail Making Test
- vitD:
-
Vitamin D
- WT:
-
Wild-type
References
-
Boison D. New insights into the mechanisms of the ketogenic diet. Curr Opin Neurol. 2017;30:187–92.
-
Vidali S, Aminzadeh Southward, Lambert B, Rutherford T, Sperl W, Kofler B, et al. Mitochondria: the ketogenic diet--a metabolism-based therapy. Int J Biochem Cell Biol. 2015;63:55–9.
-
Martin-McGill KJ, Jackson CF, Bresnahan R, Levy RG, Cooper PN. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2018;11:CD001903.
-
Di Lorenzo C, Coppola Thou, Di Lenola D, Evangelista Thou, Sirianni 1000, Rossi P, et al. Efficacy of modified Atkins ketogenic diet in chronic cluster headache: an open up-characterization, unmarried-arm, clinical trial. Front Neurol. 2018;9:64.
-
Matsuzaki T, Sasaki Yard, Tanizaki Y, Hata J, Fujimi K, Matsui Y, et al. Insulin resistance is associated with the pathology of Alzheimer disease: the Hisayama Written report. Neurology. 2010;75:764–seventy.
-
El-Lebedy D, Raslan HM, Mohammed AM. Apolipoprotein East gene polymorphism and gamble of type 2 diabetes and cardiovascular affliction. Cardiovasc Diabetol. 2016;15:12.
-
Swerdlow RH. Mitochondria and cell bioenergetics: increasingly recognized components and a possible etiologic crusade of Alzheimer'southward illness. Antioxid Redox Indicate. 2012;16:1434–55.
-
Cunnane SC, Courchesne-Loyer A, Vandenberghe C, St-Pierre V, Fortier One thousand, Hennebelle K, et al. Can ketones help rescue brain fuel supply in later life? Implications for cognitive health during aging and the treatment of Alzheimer's disease. Front Mol Neurosci. 2016;9:53.
-
Noh HS, Hah Y-S, Nilufar R, Han J, Bong J-H, Kang SS, et al. Acetoacetate protects neuronal cells from oxidative glutamate toxicity. J Neurosci Res. 2006;83:702–9.
-
Bender KJ, Wetherington J, Hassel B, Peel JF, Gawryluk JW, Greene JG, et al. Mitochondrial biogenesis in the anticonvulsant mechanism of the ketogenic diet. Ann Neurol. 2006;threescore:223–35.
-
Masino SA, Kawamura M, Wasser CD, Wasser CA, Pomeroy LT, Ruskin DN. Adenosine, ketogenic nutrition and epilepsy: the emerging therapeutic relationship betwixt metabolism and encephalon activeness. Curr Neuropharmacol. 2009;vii:257–68.
-
Kashiwaya Y, Takeshima T, Mori North, Nakashima K, Clarke Thou, Veech RL. d-β-hydroxybutyrate protects neurons in models of Alzheimer'due south and Parkinson's disease. Proc Natl Acad Sci U S A. 2000;97:5440–four.
-
Jeong EA, Jeon BT, Shin HJ, Kim N, Lee DH, Kim HJ, et al. Ketogenic diet-induced peroxisome proliferator-activated receptor-γ activation decreases neuroinflammation in the mouse hippocampus after kainic acid-induced seizures. Exp Neurol. 2011;232:195–202.
-
Broom GM, Shaw IC, Rucklidge JJ. The ketogenic diet as a potential handling and prevention strategy for Alzheimer's disease. Nutr Burbank Los Angel Cty Calif. 2019;lx:118–21.
-
Włodarek D. Role of ketogenic diets in neurodegenerative diseases (Alzheimer's disease and Parkinson's disease). Nutrients. 2019;11. https://doi.org/ten.3390/nu11010169.
-
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
-
Aso E, Semakova J, Joda L, Semak V, Halbaut 50, Calpena A, et al. Triheptanoin supplementation to ketogenic nutrition curbs cognitive damage in APP/PS1 mice used as a model of familial Alzheimer's affliction. Curr Alzheimer Res. 2013;10:290–7.
-
Beckett TL, Studzinski CM, Keller JN, Paul Murphy M, Niedowicz DM. A ketogenic nutrition improves motor functioning but does not bear upon β-amyloid levels in a mouse model of Alzheimer'due south illness. Brain Res. 2013;1505:61–7.
-
Brownlow ML, Benner Fifty, D'Agostino D, Gordon MN, Morgan D. Ketogenic diet improves motor performance merely not cognition in two mouse models of Alzheimer's pathology. PLoS One. 2013;8:e75713.
-
Hernandez AR, Hernandez CM, Campos KT, Truckenbrod LM, Sakarya Y, McQuail JA, et al. The antiepileptic ketogenic nutrition alters hippocampal transporter levels and reduces adiposity in aged rats. J Gerontol A Biol Sci Med Sci. 2018;73:450–8.
-
Hernandez AR, Hernandez CM, Campos Thousand, Truckenbrod L, Federico Q, Moon B, et al. A ketogenic diet improves cognition and has biochemical furnishings in prefrontal cortex that are dissociable from hippocampus. Front Crumbling Neurosci. 2018;10:391.
-
Kashiwaya Y, Bergman C, Lee J-H, Wan R, King MT, Mughal MR, et al. A ketone ester nutrition exhibits anxiolytic and cognition-sparing backdrop, and lessens amyloid and tau pathologies in a mouse model of Alzheimer'southward disease. Neurobiol Aging. 2013;34:1530–9.
-
Newman JC, Covarrubias AJ, Zhao M, Yu X, Gut P, Ng C-P, et al. Ketogenic diet reduces midlife mortality and improves retention in aging mice. Cell Metab. 2017;26:547–57 e8.
-
Pan Y, Larson B, Araujo JA, Lau W, de Rivera C, Santana R, et al. Dietary supplementation with medium-chain TAG has long-lasting cognition-enhancing effects in anile dogs. Br J Nutr. 2010;103:1746–54.
-
Pawlosky RJ, Kemper MF, Kashiwaya Y, Rex MT, Mattson MP, Veech RL. Effects of a dietary ketone ester on hippocampal glycolytic and tricarboxylic acid cycle intermediates and amino acids in a 3xTgAD mouse model of Alzheimer'due south disease. J Neurochem. 2017;141:195–207.
-
Van der Auwera I, Wera Southward, Van Leuven F, Henderson ST. A ketogenic diet reduces amyloid beta 40 and 42 in a mouse model of Alzheimer'southward disease. Nutr Metab. 2005;2:28.
-
Wang D, Mitchell ES. Cognition and synaptic-plasticity related changes in anile rats supplemented with eight- and 10-carbon medium chain triglycerides. PLoS One. 2016;11:e0160159.
-
Fortier M, Castellano C-A, Croteau Eastward, Langlois F, Bocti C, St-Pierre V, et al. A ketogenic beverage improves brain energy and some measures of cognition in mild cognitive damage. Alzheimers Dement J Alzheimers Assoc. 2019;15:625–34.
-
Ota G, Matsuo J, Ishida I, Takano H, Yokoi Y, Hori H, et al. Furnishings of a medium-chain triglyceride-based ketogenic formula on cognitive function in patients with mild-to-moderate Alzheimer'due south disease. Neurosci Lett. 2019 Jan 18;690:232–six.
-
Torosyan North, Sethanandha C, Grill JD, Dilley ML, Lee J, Cummings JL, et al. Changes in regional cerebral claret flow associated with a 45 twenty-four hour period form of the ketogenic amanuensis, caprylidene, in patients with mild to moderate Alzheimer's disease: results of a randomized, double-blinded, pilot study. Exp Gerontol. 2018;111:118–21.
-
Taylor MK, Sullivan DK, Mahnken JD, Burns JM, Swerdlow RH. Feasibility and efficacy data from a ketogenic nutrition intervention in Alzheimer'southward disease. Alzheimers Bewilder North Y N. 2018;iv:28–36.
-
Abe Southward, Ezaki O, Suzuki M. Medium-chain triglycerides in combination with leucine and vitamin D do good cognition in frail elderly adults: a randomized controlled trial. J Nutr Sci Vitaminol (Tokyo). 2017;63:133–40.
-
Ota M, Matsuo J, Ishida I, Hattori K, Teraishi T, Tonouchi H, et al. Consequence of a ketogenic repast on cognitive role in elderly adults: potential for cognitive enhancement. Psychopharmacology. 2016;233:3797–802.
-
Ohnuma T, Toda A, Kimoto A, Takebayashi Y, Higashiyama R, Tagata Y, et al. Benefits of use, and tolerance of, medium-chain triglyceride medical food in the management of Japanese patients with Alzheimer'due south disease: a prospective, open-characterization pilot study. Clin Interv Aging. 2016;eleven:29–36.
-
Rebello CJ, Keller JN, Liu AG, Johnson WD, Greenway FL. Pilot feasibility and safety report examining the effect of medium concatenation triglyceride supplementation in subjects with mild cognitive impairment: a randomized controlled trial. BBA Clin. 2015;3:123–5.
-
Krikorian R, Shidler MD, Dangelo One thousand, Couch SC, Benoit SC, Clegg DJ. Dietary ketosis enhances memory in mild cognitive impairment. Neurobiol Aging. 2012;33:425 e19–27.
-
Henderson ST, Vogel JL, Barr LJ, Garvin F, Jones JJ, Costantini LC. Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer'southward disease: a randomized, double-blind, placebo-controlled, multicenter trial. Nutr Metab. 2009;six:31.
-
Reger MA, Henderson ST, Hale C, Cholerton B, Baker LD, Watson GS, et al. Effects of beta-hydroxybutyrate on cognition in retentiveness-impaired adults. Neurobiol Aging. 2004;25:311–4.
-
Huang Q, Ma S, Tominaga T, Suzuki K, Liu C. An viii-week, low carbohydrate, high fat, ketogenic diet enhanced exhaustive practise capacity in mice office two: effect on fatigue recovery, post-practise biomarkers and anti-oxidation capacity. Nutrients. 2018;ten. https://doi.org/x.3390/nu10101339.
-
Ma S, Huang Q, Tominaga T, Liu C, Suzuki Yard. An 8-week ketogenic diet alternated interleukin-6, ketolytic and lipolytic factor expression, and enhanced exercise capacity in mice. Nutrients. 2018;10. https://doi.org/10.3390/nu10111696.
-
Ma S, Huang Q, Yada M, Liu C, Suzuki K. An 8-calendar week ketogenic low carbohydrate, high fat diet enhanced exhaustive exercise chapters in mice. Nutrients. 2018;10. https://doi.org/10.3390/nu10060673.
-
Wang J, Ho Fifty, Qin Westward, Rocher AB, Seror I, Humala N, et al. Caloric restriction attenuates beta-amyloid neuropathology in a mouse model of Alzheimer'south disease. FASEB J Off Publ Fed Am Soc Exp Biol. 2005;nineteen:659–61.
-
Hall AM, Roberson ED. Mouse models of Alzheimer's disease. Encephalon Res Bull. 2012;88:3–12.
-
Bolla AM, Caretto A, Laurenzi A, Scavini Chiliad, Piemonti L. Low-carb and ketogenic diets in type 1 and type 2 diabetes. Nutrients. 2019;xi. https://doi.org/10.3390/nu11050962.
-
Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Brehm BJ, et al. Effects of depression-saccharide vs low-fat diets on weight loss and cardiovascular run a risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166:285–93.
-
Castellano C-A, Nugent Southward, Paquet North, Tremblay S, Bocti C, Lacombe G, et al. Lower brain 18F-fluorodeoxyglucose uptake merely normal 11C-acetoacetate metabolism in mild Alzheimer's disease dementia. J Alzheimers Dis JAD. 2015;43:1343–53.
-
Martínez-Lapiscina EH, Galbete C, Corella D, Toledo E, Buil-Cosiales P, Salas-Salvado J, et al. Genotype patterns at CLU, CR1, PICALM and APOE, cognition and Mediterranean diet: the PREDIMED-NAVARRA trial. Genes Nutr. 2014;9:393.
-
Mehta D, Jackson R, Paul Chiliad, Shi J, Sabbagh Chiliad. Why do trials for Alzheimer's affliction drugs continue failing? A discontinued drug perspective for 2010-2015. Proficient Opin Investig Drugs. 2017;26:735–nine.
-
Sanders CL, Wengreen HJ, Schwartz Southward, Behrens SJ, Corcoran C, Lyketsos CG, et al. Nutritional status is associated with severe dementia and mortality: the Cache Canton Dementia Progression Study. Alzheimer Dis Assoc Disord. 2018;32:298–304.
Acknowledgements
Not applicable.
Author information
Affiliations
Contributions
ML and BP analysed and interpreted the data and drafted the manuscript. EC, JH and FML critically reviewed the selected studies and revised the manuscript appropriately. CP conceived the original thought, reviewed the selected studies and revised the last version of the manuscript. All authors read and approved the submitted version.
Corresponding writer
Ethics declarations
Ethics blessing and consent to participate
Non applicative.
Consent for publication
Not applicative.
Competing interests
The authors declare that they have no competing interests.
Boosted data
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits utilize, sharing, accommodation, distribution and reproduction in whatever medium or format, as long as you give advisable credit to the original author(due south) and the source, provide a link to the Creative Commons licence, and point if changes were made. The images or other third party material in this article are included in the article'southward Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article'due south Artistic Commons licence and your intended employ is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a re-create of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this commodity
Cite this article
Lilamand, M., Porte, B., Cognat, E. et al. Are ketogenic diets promising for Alzheimer's disease? A translational review. Alz Res Therapy 12, 42 (2020). https://doi.org/10.1186/s13195-020-00615-4
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s13195-020-00615-4
Keywords
- Ketogenic diet
- Alzheimer's disease
- Encephalon metabolism
- Brute models
sleemanthriasself.blogspot.com
Source: https://alzres.biomedcentral.com/articles/10.1186/s13195-020-00615-4

0 Response to "Systematic Review of Ketogenic Diet and Cognitive Disorders"
Post a Comment